I’ve spent time during the past year or so approaching my colleagues and asking, “What percentage of our patients do you think will be sober/clean in a year?” I varied my delivery: Sometimes I used “sober,” sometimes “clean.” At times I said “alcoholics,” and other times I said “addicts.” It clearly was an informal survey. I presented the question to people with whom I work directly, as well as to friends and colleagues working at other treatment centers. I wasn’t entirely surprised when I got responses such as “50 percent,” or even “10 percent.”
 It became clear to me that a lot of the professionals with whom I work on a daily basis seem to believe that treatment for substance use disorders (SUDs) is not very effective.
It became clear to me that a lot of the professionals with whom I work on a daily basis seem to believe that treatment for substance use disorders (SUDs) is not very effective.
I had begun to make this inquiry because I had been growing tired of friends and neighbors asking me questions that clearly conveyed their impression that treating SUDs is a waste of time. It’s hard to blame them. My local newspaper and television stations in South Florida are constantly reporting about scams in our industry. Celebrities get a lot of coverage when they hit bottom or start using again. Success stories do not receive that kind of attention. Moreover, those of us who have achieved long-term recovery often remain silent.
Changing cultural beliefs may take time. To some extent, we’re powerless over them. However, there are some factors that we can control. Why do many professionals treating SUDs have the perception that treatment has such a limited impact? There clearly is strong evidence that treatment is very effective when a plan for recovery is followed.
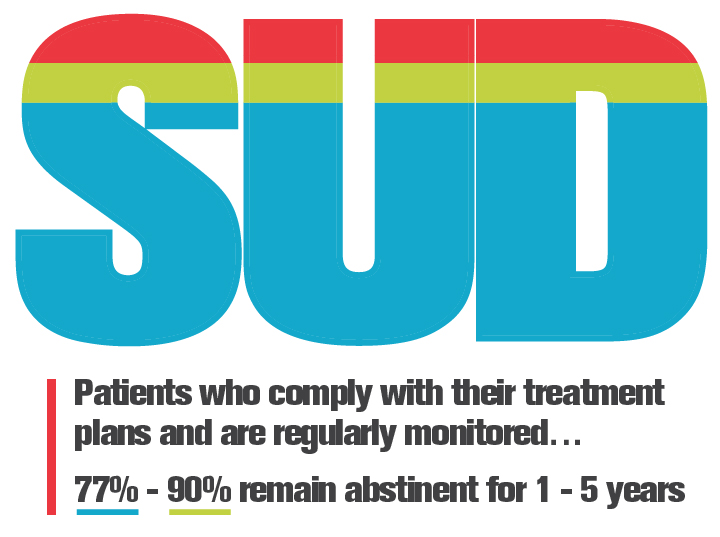
Studies have demonstrated that 77 to 90 percent of patients who comply with their treatment plans and are regularly monitored remain abstinent for periods of one to five years. (1, 2, 3, 4) Why do people who work as addiction professionals not know this? Why is this not regularly conveyed to patients in treatment? It can serve as a motivator. The effectiveness of treatment for SUDs when patients follow an extended-care plan is gratifying.
Concern in first year
However, as a profession, we come face to face with another problem. Many patients who do not follow an extended-care plan become unstable during their first year into recovery. A frequently cited study published in 2000 indicates that 40 to 60 percent of patients who have completed residential care for a SUD become unstable during their first year in recovery. (5)
However, patients with other chronic diseases such as asthma, Type II diabetes and hypertension become unstable at similar rates. So why do people, generally speaking, not have a similarly glum expectation when it comes to the effectiveness of treatment for the other chronic diseases?
One possibility is that it is commonly recognized that patients being treated for other chronic diseases will always be in treatment. Their treatment plans extend for a lifetime. Professionals and non-professionals alike accept that diabetics will always have difficulty keeping their blood sugar stable, asthmatics will always have respiratory problems and the blood pressure of patients with hypertension will occasionally become elevated.
Treatment cannot be perceived as unsuccessful for patients with other chronic diseases because they are still in treatment. People with SUDs are perceived to have completed treatment. It’s over! The SUD was treated as an acute occurrence.
Diseases treated with an acute-care model are curable. Patients and the public expect a cure. When people with SUDs become unstable, the acute care they received is seen as having been ineffective.
I think most addiction professionals believe that we treat a chronic disease. Personally, I have only recently realized that we have been using an acute-care mode. I wish I could say that it was my discovery. But authorities, such as William White, have been making this point for some time. (6) Change never comes easily or quickly.
Measuring effectiveness
 If we want to evolve toward treating SUDs as a chronic disease, there are ways to begin. (4, 7) As we move toward a chronic-care model, we want to measure the effectiveness of what we do in a manner similar to measuring the impact of protocols for other chronic diseases. (8) The ways we have been measuring treatment effectiveness are about as insane as the disease we treat.
If we want to evolve toward treating SUDs as a chronic disease, there are ways to begin. (4, 7) As we move toward a chronic-care model, we want to measure the effectiveness of what we do in a manner similar to measuring the impact of protocols for other chronic diseases. (8) The ways we have been measuring treatment effectiveness are about as insane as the disease we treat.
Traditionally, we have used total abstinence as a measure of treatment effectiveness. In the past, the patient who completed residential care, had a weekend recurrence a few months down the road and soon returned to abstinence has been considered “unsuccessful.” The measure of treatment effectiveness that we have chosen is perfection. Maybe, we should instead be measuring sustained action in the pursuit of abstinence. (9) A patient who continues to have his/her addictive disease treated is never unsuccessful.
Need to change how we measure the effectiveness of treatment.
After all, what would the success rate be for diabetes if the only measure of treatment effectiveness were perfectly stable blood sugar levels?
Perhaps, a good definition of a patient taking sustained action in the pursuit of abstinence is continued engagement in a recovery-oriented system of care (ROSC). (10) ROSCs can include the contributions of coaches, interventionists, outpatient resources, physicians, private therapists, and residential extended-care operations, among others. The person engaged with a ROSC remains in the process of getting well.
This resembles a person with hypertension continuing to work with a nutritionist and a physician to get his/her blood pressure under control. The patient having his/her hypertension treated is not unsuccessful. Neither is the person pursuing consistent abstinence from substances.
Certainly, mine is not the only call for a chronic-care model, and the need to change how we measure the effectiveness of treatment. I might be one of few saying that we need to take responsibility for how we are perceived. Has anyone ever seen professionals who treat other chronic diseases work as hard as we do to convince ourselves and the public that “treatment works?” I look forward to the day when we won’t have to.




Leave a Reply
You must be logged in to post a comment.