In an effort counteract rampant, nationwide prescription drug abuse, the Food and Drug Administration has announced approval of a new extended-release form of oxycodone. The new pill is called Targiniq ER, and was developed with an abuse-deterrent formula. It is one of only two opioid painkillers approved by the FDA to list its deterrent properties on the label.
The drug is comprised of oxycodone and naloxone, a drug commonly used to treat overdose victims. Approval comes with restrictions; the FDA has said that Targiniq ER should only be prescribed to patients who can’t find relief from other pain medications. The approval was outlined in a recent article and could be a significant clinical step toward curbing prescription painkiller abuse.[1]
The FDA claims that Targiniq ER will work to deter abuse, but will not totally prevent it. In the event of the drug being snorted or injected (preferred forms of abuse because of their fast-acting effects), the naloxone in Targiniq ER will kick in to block the pleasurable effects that would ordinarily travel to the brain’s receptors. Targiniq ER will be marketed by Purdue Pharma. The FDA has also granted Purdue priority review designation for a pure form of hydrocodone painkiller, which also has an abuse-deterrent formula.
FDA Hopes New Prescription Opioid Will Diminish Risk
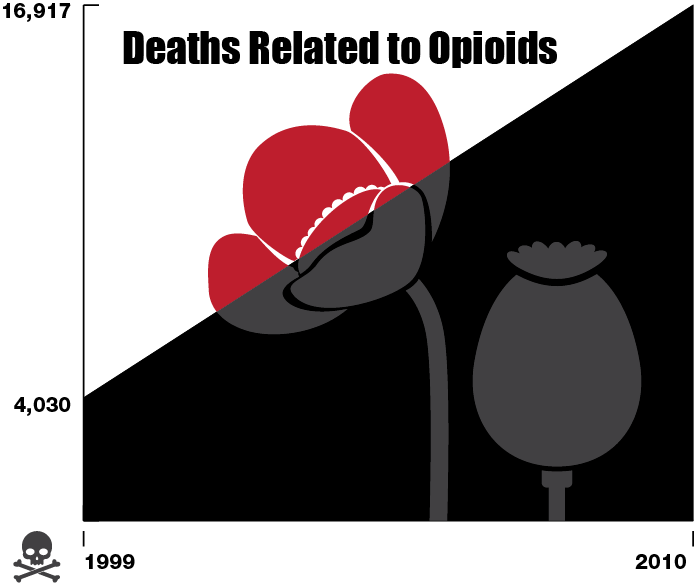
The FDA is being pulled in several different directions and is facing intense public and political pressure to address both the nation’s rising opioid overdose rates and the 100 million Americans struggling with chronic pain. In 2010, there were enough painkillers prescribed in the U.S. to medicate every adult in the country, 24 hours per day for a month.Since 1999, the amount of annual deaths related to opioids has skyrocketed from 4,030 to 16,917. The CDC estimated that abuse of opioids (which includes heroin) killed 110 Americans per day in 2011, with opioid pain relievers being involved in more than half of the 41,300 recorded drug poisonings that year.[2]
Targiniq ER blocks the euphoric effects of opioids, making it a less desirable option for abuse, though the FDA warned that the drug can still be abused. The safety and effectiveness of the drug were tested in a clinical trial involving 600 people with chronic lower back pain. The deterrent features were evaluated through studies on more than 3,000 people. Side effects include nausea and vomiting, most commonly.
Analyzing America’s Opioid Abuse Problem

There are more fatal overdoses from prescription painkillers in the U.S. than from cocaine and heroin combined, according to the CDC. Prescriptions for painkillers have nearly tripled in the past 20 years, and opioid pain reliever overdose deaths have quadrupled since 1999. The CDC has declared the problem of prescription painkiller abuse a national health epidemic.
Increases in the prescribing of drugs like oxycodone, hydrocodone, fentanyl and methadone are the driving force in the rise of opioid abuse. Prescriptions began rising in the 1990s, when physicians were attempting to address the perceived widespread problem of untreated or undertreated pain. Now, the supply of opioids has grown out of control.
An international study by the British medical journal, The Lancet, found that wealthy nations such as the U.S., the United Kingdom and Australia were the most vulnerable to opioid abuse. The study showed people in these countries had abuse rates 20 times higher than in the least effected countries.
Pressure is on Government to Do More
 Whether you point the finger at doctors needing to be more cautious in prescribing drugs, the FDA for failing to regulate them more effectively or at the federal government for failing to create higher access to affordable drug treatment, it’s clear that something must be done to curb this health crisis.
Whether you point the finger at doctors needing to be more cautious in prescribing drugs, the FDA for failing to regulate them more effectively or at the federal government for failing to create higher access to affordable drug treatment, it’s clear that something must be done to curb this health crisis.
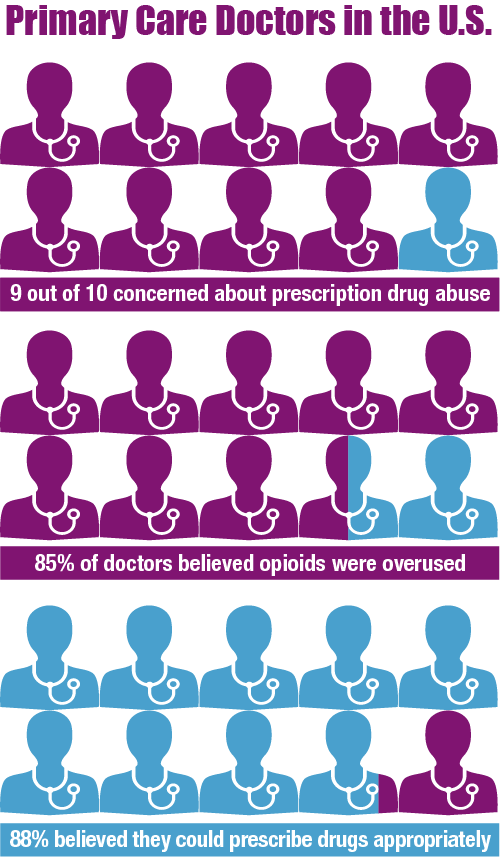
Doctors are in difficult positions because they want to give their patients relief from pain, but don’t want to promote abuse or addiction. Nine out of 10 primary care doctors in the U.S. said they were concerned about prescription drug abuse and were less likely to prescribe them than they were a year ago, according to a 2014 research letter published in JAMA Internal Medicine. As part of the same research, they found that 85 percent of doctors believed that opioids were overused. Despite all of that, 88 percent believed they could prescribe drugs appropriately.
Another fact to consider is that despite the increase in opioid abuse and addiction, only a small portion of those who do need help actually receive it. Reasons for failing to seek or receive treatment include unavailability, a lack of resources, unwillingness to accept addiction treatment, or complete ignorance or blindness to the problem.
The FDA has also received some criticism for its role in the problem. Dr. Andrew Kolodny, president of Physicians for Responsible Opioid Prescribing, has put the onus on the FDA to change its labeling requirements to make them more specific and allow doctors to prescribe more prudently. Kolodny said there are limited guidelines on maximum dosages and suggested duration of use, and that the drugs should be limited to people suffering from “severe pain,” not the current standard of “moderate to severe pain.”
Nationwide Education on Drug-Free Pain Management Needed
At the heart of this issue is the general belief that the only treatment for acute and chronic pain are painkillers. While over the counter and prescription drugs do offer immediate pain relief in most situations, there are multiple issues to be concerned with when pill use is prolonged. Increased tolerance leads patients to use more pills in an effort to find relief, which often ends in dependence and possibly addiction.
Additionally, and most importantly, pain pills do not target the source of pain, so they only serve as temporary relief. Once the effect of the pills wear off, the pain returns and the cycle restarts. It’s for this reason that the public needs to be educated about drug-free pain management techniques.
A simple change to a person’s diet, an improvement in their fitness, some flexibility training and many other methods can naturally reduce a person’s pain to manageable levels over time. While pain medication is necessary for immediate relief and for cases of severe pain, all patients should concurrently be exploring and be educated about drug-free options to avoid long-term health complications.